Dr. Michael Wilderman is among only a few physicians in the region to have access to the first and only commercially available branched device to treat thoracic aortic conditions
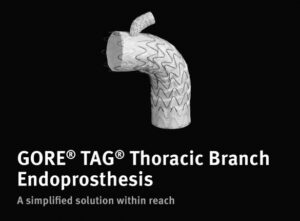 News Release/HACKENSACK, NJ – On August 16, 2022, Michael Wilderman, M.D., chief of Endovascular Surgery at Hackensack Meridian Hackensack University Medical Center, became the first in the U.S. to perform a commercial minimally invasive repair of a Type B aortic dissection using the new GORE® TAG® Thoracic Branched Endoprosthesis (TBE) — marking the first time the device was implanted at a non-clinical trial site.
News Release/HACKENSACK, NJ – On August 16, 2022, Michael Wilderman, M.D., chief of Endovascular Surgery at Hackensack Meridian Hackensack University Medical Center, became the first in the U.S. to perform a commercial minimally invasive repair of a Type B aortic dissection using the new GORE® TAG® Thoracic Branched Endoprosthesis (TBE) — marking the first time the device was implanted at a non-clinical trial site.
Cynthia (Cindy) Pecorelli, 62, of Belleville, New Jersey, was the recipient of the TBE.
“A few days after July 4, I felt severe pain in my upper abdomen and back — probably an eight or nine on a scale of 1-10,” said Cynthia. “It slowly went away, but when I went to the doctor the next day, he sent me to the emergency room.”
Cynthia was transferred from her local hospital to Hackensack University Medical Center, where Emergency Department physicians performed a CT scan, bloodwork and an ultrasound to diagnose her with a Type B thoracic aortic dissection. A Type B thoracic aortic dissection happens when a tear occurs in the inner layer of the portion of the aorta — the body’s main artery — that descends from the heart into the chest.
Innovative Treatment Options for a Complex Condition
Aortic dissection is a life-threatening condition that requires emergency evaluation and expert treatment. Dr. Wilderman is one of the most experienced physicians in the country in the treatment of aortic conditions, presenting his research at national and international meetings and training other physicians on the latest treatment approaches.
He offers a full range of treatment options for aortic conditions, with a focus on developing and utilizing innovative minimally invasive techniques to treat patients who are unable to undergo traditional open aortic repair surgery. As a result, Hackensack University Medical Center is a regional destination for comprehensive care of aortic conditions.
“As an early adopter who is expertly trained in the latest minimally invasive techniques to treat aortic dissection, Dr. Wilderman is one of the first physicians in the region to have access to the innovative Gore TBE device — which is the first and only commercially available, ‘off-the-shelf’ device designed to provide minimally invasive treatment of thoracic aortic conditions,” said Gregory Simonian, M.D., director of the Cardiovascular Center of Excellence at Hackensack University Medical Center.
During the procedure, the TBE is inserted through a small incision in the groin. The TBE has a pre-made fenestration – or hole – that allows it to be placed across the arch of the aorta in the chest while still preserving blood flow to the branched artery that supplies the arm, brain and spinal cord.
Before the approval of the Gore device, surgeons either needed to perform a major bypass procedure to maintain blood flow to the arm, brain and spinal cord, or temporarily cut off blood flow altogether, which increases the risk of stroke. As a result, two operations were required to repair the dissection and restore blood flow to the branched artery. And although custom-made devices were available, they often took 4-5 weeks to make — which was too long of a wait for patients who needed emergency treatment.
“The Gore TBE contributes to improved outcomes by reducing operative time, length of stay and patient discomfort,” said Dr. Wilderman. “We can now treat thoracic aortic aneurysms using a single device in a single surgery performed through two small incisions in the groin and one in the wrist — with immediate access to the device, and without the need for open surgery.”
Minimally Invasive Care Delivers Outstanding Outcome
After stabilizing Cynthia’s condition during her Emergency Department visit, Dr. Wilderman determined that Cynthia did not need emergency treatment. Evidence showed the safest option was to allow Cynthia’s delicate aorta to “rest” for a few weeks to reduce the risk of complications during the aortic dissection repair.
“Performing surgery too soon or too late can lead to poor outcomes,” said Dr. Wilderman. “We have the experience to identify the optimal time to perform a procedure and the best approach to use for each patient.”
On August 16, 2022, Dr. Wilderman — in collaboration with Dr. Simonian and vascular and cardiac surgery colleagues — performed Cynthia’s procedure at Hackensack University Medical Center.
“In Cynthia’s case, Dr. Wilderman and his team applied experience, clinical evidence and effective initial assessment and treatment to optimize the patient before surgery,” said Dr. Simonian. “The team was able to convert an emergency to a semi-elective procedure, which provided outstanding results.”
“Cynthia went home the day after surgery and did very well,” said Dr. Wilderman. “With the support of a multidisciplinary team of cardiovascular experts, we were able to perform a ‘first-of-its-kind’ procedure right here in New Jersey, meaning that Cynthia didn’t have to travel far to receive the life-saving care she needed.”
“We are proud to have the expertise and access to the latest technology that allows us to offer our patients the latest treatment options — especially for a complex, life-threatening condition like aortic dissection,” said Mark Sparta, FACHE, president, Northern Region, and president and chief hospital executive, Hackensack University Medical Center. “We are a regional referral center for aortic dissection treatment, and we want our patients and referring physicians to know that they can trust us to offer the most advanced care.”
“Dr. Wilderman and our team members are among the nation’s leaders in treating complex aortic conditions, which means that Cynthia and others who develop this condition can turn to us for an accurate diagnosis, a comprehensive care plan and innovative treatment options,” said Ihor S. Sawczuk, MD, FACS, Hackensack Meridian Health’s president of Academics, Research and Innovation, and also associate dean of Clinical Integration and professor and chair emeritus of Urology at the Hackensack Meridian School of Medicine..
“I was a little nervous about the procedure, but Dr. Wilderman was very reassuring. He explained exactly what happened and what he was going to do to fix it. After the procedure was done, I had no pain at all — and 10 days later, I’m back to normal,” said Cynthia. “I knew I was in good hands with Dr. Wilderman, and I’m glad he was the one who performed my procedure. God bless Dr. Wilderman and his team.”







